The Surgical Outcome Risk Tool (SORT) – a preoperative risk prediction tool
The SORT is a FREE preoperative risk prediction tool that provides a percentage risk for mortality within 30 days of surgery. Developed and validated on a UK adult patient population (aged 16 or over) who had surgery as part of an inpatient stay. Exclusions: obstetrics, neurosurgery, cardiac, and transplant surgery.
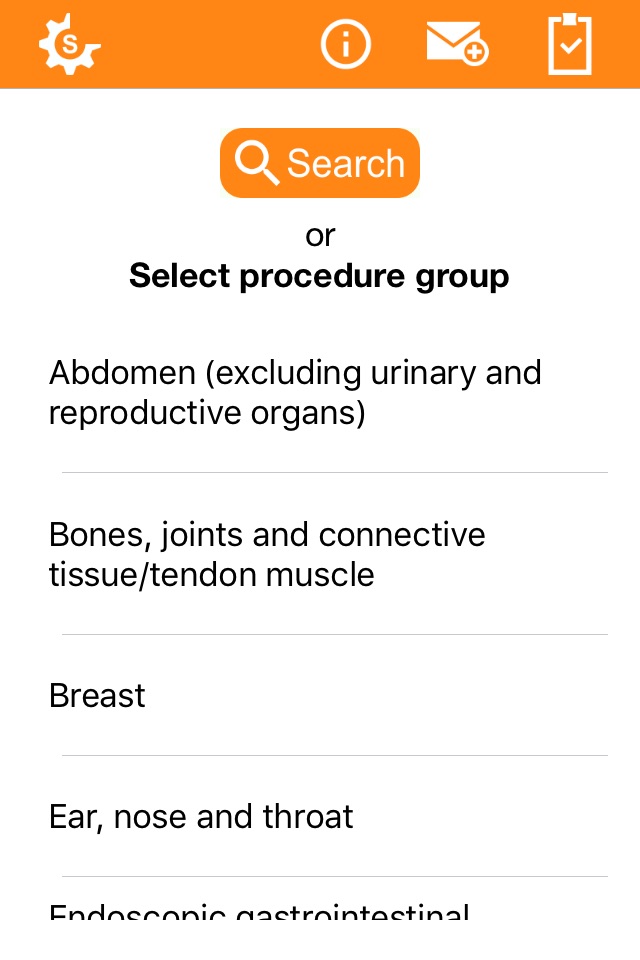
FEATURES:
* Offline capability - this means the calculator works even where there is no mobile/wireless reception, for example in all clinical settings and even in reception black spots.
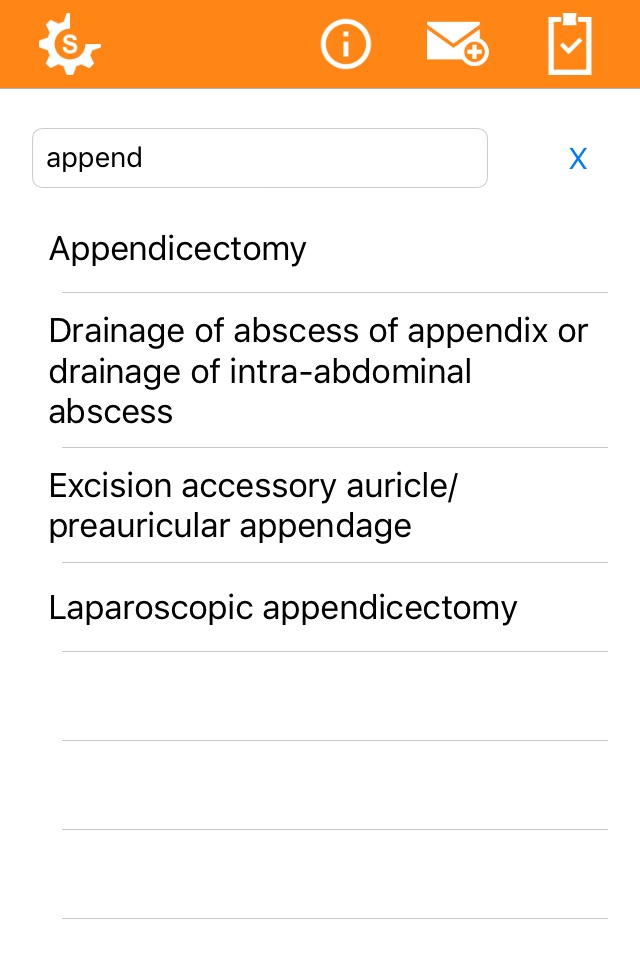
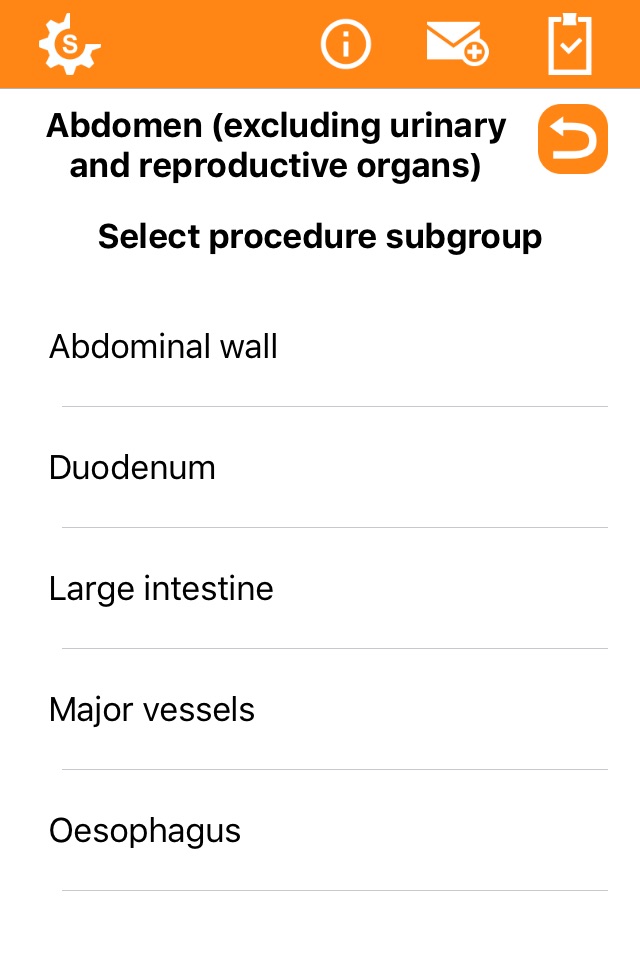
* Includes a DYNAMIC search button for a free text search of surgical procedures;
* All variables are quick and easy to obtain before surgery, giving the SORT an advantage over some other widely-available risk assessment tools;
* Can be used for all surgical severity from minor-complex categories of surgery;
* For all surgical urgency from elective to immediate/emergency surgery;
POTENTIAL AREAS OF USE:
* There is an increased focus on peri-operative medicine including risk assessments of patients and potential outcomes following surgery.
* The SORT provides a mortality estimate that can help set the scene to identify high risk patients, who might benefit from interventions such as admission to critical care. It could also contribute to preoperative assessments, the consent process and shared decision-making with patients and aid resource planning.
* A simple tool that could be used together with clinical judgement and as part of the overall surgical toolkit.
* From a survey we know that the SORT is starting to be used in pre-assessment clinics, high risk clinics, emergency departments, and surgery departments.
BACKGROUND:
* Developed by researchers from The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) - and doctors from the UCL/UCLH Surgical Outcomes Research Centre (SOuRCe);
* A high ranking journal. The work was published in the British Journal of Surgery in 2014;
* A large data set. Following exclusions from 19,097 anonymised patient records from an NCEPOD study, from 326 NHS and independent sector hospitals in the UK, 16,788 records were used in the analyses;
* A large scale study. At the time of publication, this work represented the largest analysis of risk prediction tools in a UK cohort of patients undergoing inpatient surgery in multiple surgical specialties.
We hope this software tool proves to be a useful addition to your overall surgical toolkit.